From animals to environment: How livestock antibiotic use drives human health risks beyond the farm
Antibiotics are essential for keeping livestock healthy, especially in fast-growing sectors like chicken and pig farming. But what happens when they are administered and excreted? A new study on ‘Antibiotic ecotoxicity and resistance risks in resource-constrained chicken and pig farm environments’ by researchers at the International Livestock Research Institute (ILRI) traces how antibiotics from farms enter the environment, revealing risks to both public health and ecosystems, particularly in resource-constrained settings like Kenya.
By analyzing farm practices like antibiotic use and manure management, and linking this data to antibiotic levels found in manure, compost and soil, the study offers a crucial look at the scale of antibiotic pollution and its potential to fuel antimicrobial resistance (AMR) – often called a "silent pandemic".
Between April and July 2022, the researchers surveyed 97 chicken and pig farms in Kenya's Kajiado and Kiambu counties, adjacent to Nairobi. They zeroed in on eight common veterinary antibiotics, including those with familiar names like tetracycline, oxytetracycline, sulfamethoxazole and trimethoprim.
While the average antibiotic concentration across all environmental samples was relatively low at 63.4 micrograms per kilogram (µg/kg), some concerning levels were found. Trimethoprim, in particular, exceeded the environmentally relevant threshold of 100 µg/kg with an average of 212.4 µg/kg, and soils fertilized with pig manure also surpassed this limit, averaging 129.3 µg/kg. Antibiotics were frequently detected in chicken compost (25.8% of samples) and pig manure-fertilized soils (23.1% of samples). Among the individual antibiotics, sulfamethoxazole was detected most often, followed by tylosin and tetracycline.

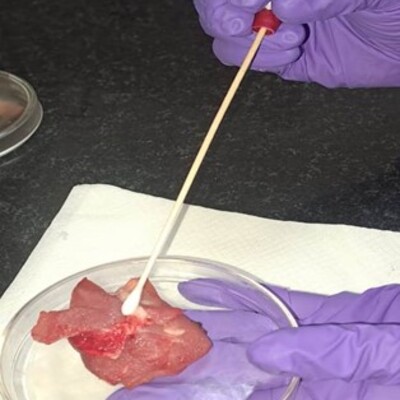
Sample collection in a chicken farm to assess drivers of antimicrobial use in poultry. (photo credit; ILRI/Pamela Wairagala).
Assessing the risk: Low, but not zero
To understand the potential environmental impact of these results, the researchers calculated ‘risk quotients’ (RQ) – a way to measure the likelihood of harm. Generally, the study found low risks for both ecotoxicity (harm to the environment itself) and antimicrobial resistance (AMR) selection (promoting the growth of resistant bacteria), both often scoring below the high-risk threshold of 1 (or below 0.1 for low risk).
But these risks were not uniform and showed a clear pattern: risk levels tended to climb with increasing farm size and the number of different antibiotics used on the farm. Pig farms, especially, showed higher AMR risks compared to chicken farms. Farm practices, including the size of the herd or flock, how many types of antibiotics were used, and how manure was managed and stored, were identified as key factors influencing these risks. This connection highlights how decisions by livestock farmers can have impacts that stretch far beyond the farm gates, potentially even affecting the health of crops grown in contaminated soil.
Farmers speak out: Challenges and concerns
Fredrick Gudda, the lead author of the study and a former PhD fellow at ILRI's One Health Research, Education, and Outreach Centre in Africa (OHRECA), pointed out that some farmers rely heavily on antibiotics for disease prevention without fully grasping the wider issue of AMR. To bridge this gap, after the study, Gudda and other experts held awareness raising sessions with farmers and veterinary professionals in the two counties.
These discussions brought farmers’ concerns to the forefront. Some said that regular antibiotic use is necessary throughout the production cycle. Others highlighted practical challenges such as ‘veterinary personnel are expensive and unavailable,’ which leads farmers to rely on advice from peers or their own experience to self-administer drugs. A key question raised was why seemingly problematic antibiotic combinations are still readily available in local veterinary shops. ‘If these are risky, why are they sold openly?’
Animal health experts at the sessions addressed these points, explaining the dangers of using multi-ingredient antibiotic products and stressing the need to reserve certain critical antibiotics, like colistin, for human health. They underscored that misuse of antibiotics can lead to longer treatment times, financial losses and the spread of resistant bacteria between farms.

Fredrick Gudda the lead author conducts awareness sessions with farmers to address the misuse of antibiotics in livestock production and the growing threat of antimicrobial resistance (AMR) (photo credit; ILRI/).
Pathways to progress: Recommendations and global action
Based on their findings and discussions, the ILRI researchers offered practical recommendations to farmers:
- Reduce reliance on antibiotics by focusing on good hygiene, better animal nutrition, and strong biosecurity measures to keep diseases out.
- Always consult qualified veterinary professionals for accurate diagnosis and appropriate treatment plans.
- Maintain detailed records of animal diseases and treatments to track antibiotic use effectively.
- Manage and treat manure to optimize decomposition and antibiotic residue degradation prior to field application.
- Participate in training workshops to stay informed about best practices in animal husbandry.
The study's results, which are published in npj Antimicrobials and Resistance, also provide valuable evidence for policymakers to develop stronger regulations that tackle environmental AMR. Aligning national efforts with global commitments, such as those from the September 2024 United Nations General Assembly High-Level Meeting on AMR, which explicitly recognized the environment as a key driver of antimicrobial resistance, is essential. There is need to strengthen regulatory frameworks to control antibiotic discharge from agricultural and livestock production, promote proper manure management and wastewater treatment in farms to minimize environmental contamination, and enhance surveillance and monitoring systems to track AMR risks in environmental reservoirs, including soil and water sources.
By adopting a One Health approach, which recognizes the interconnectedness of human, animal, and environmental health, stakeholders can work together to ensure that farming practices support not just the economy, but also public health and a sustainable environment for all. This research provides crucial insights and a valuable evidence base that serves as a vital step in understanding and addressing environmental AMR risks in critical farming regions in countries like Kenya.
This study was funded by the German Federal Ministry for Economic Cooperation and Development (BMZ) through OHRECA, led by ILRI, and the CGIAR Initiative on Protecting Human Health through a One Health Approach.
Download the full article.
You may also like
Related Publications

Patterns and factors influencing antibiotic use among poultry farmers in Thai Nguyen province, Vietnam
- Kemunto, Naomi P.
- Sinh Dang-Xuan
- Yen Luu-Thi-Hai
- Huyen Nguyen-Xuan
- Ibayi, Eugine L.
- Nielsen, S.S.
- Hung Nguyen-Viet
- Moodley, Arshnee
- Muloi, Dishon M.

Analysis of antibiotic use, biosecurity and mortality in semi-intensive broiler farms in Kenya
- Kemunto, Naomi P.
- Muloi, Dishon M.
- Ibayi, Eugine L.
- Njaramba, Jane K.
- Hoffmann, Vivian
- Murphy, Mike
- Nielsen, S.S.
- Moodley, Arshnee

Prevalence and antimicrobial-resistant Campylobacter jejuni and Campylobacter coli in free-range chickens in northwest Ethiopia
- Worku, M.
- Tessema, B.
- Ferede, G.
- Ochieng, Linnet
- Leliso, S.A.
- Mutua, Florence
- Moodley, Arshnee
- Gelaw, B.
- Grace, Delia
Prevalence and antimicrobial resistance in enterococci isolated from semi-intensive and free-range poultry farms in peri-urban Wakiso and rural Soroti, Uganda
- Ochieng, Linnet
- Ayebare, Dreck
- Ndoboli, Dickson
- Mbatidde, Irene
- Tenhagen, B.-A.
- Roesel, Kristina
- Wampande, E.
- Moodley, Arshnee

Isolation and characterization of bacteriophages with lytic activity against multidrug-resistant non-typhoidal Salmonella from Nairobi City county, Kenya
- Mugo, M.
- Musyoki, A.
- Makumi, Angela
- Mutai, I.
- Kering, K.
- Muturi, P.
- Kebenei, C.
- Weber, K.
- Pietsch, M.
- Pilz, T.
- Drechsel, O.
- Hoffmann, T.
- Wieler, L.
- Mbae, C.
- Flieger, A.
- Kariuki, S.